'One-size fits all' no longer applies to the world of pharmaceuticals. A growing understanding of genetics, the immune system and the potential for stem cells means more effective treatments and cures for severe diseases.
Today, personalized medicine is already significantly advanced. Research now shows that with generic medicine, some patients benefit, others obtain no effect at all and some even experience adverse effects. The ability to differentiate treatment between patients – even patients with the same disease – is drastically changing the pharmaceutical drug landscape. And in doing so, it has shifted the way medicines are manufactured.
One example of tailored therapies for individuals are “autologous therapies” – where a unique patient is treated with her/his own unique in vitro modified T-cells. Autologous oncology therapies are a major game changer. For example, chimeric antigen receptor cell therapy (CAR-T) initiates a bioengineered immune system attack on cancer. A groundbreaking moment in the development of these drugs was when the FDA approved Novartis Kymriah CTL019 in August 2017, the first gene therapy to treat pediatric and young adult patients with B-cell acute lymphoblastic leukemia (ALL).
The FDA has approved clinical trials for advanced therapy medicinal products (ATMPs), and now 13 cell therapies are officially approved. In fact, Donovan Jones from IIR Life sciences predicts that “The global market for cell-based therapies is expected to surpass $20 billion USD by 2025, with an annual growth rate of 21%.”
Although this new paradigm may not completely replace larger manufacturing operations, this shift in operations and manufacturing is here to stay. At this stage there is not yet an all-in-one package for a sustainable and future proof manufacturing concept, but manufacturing equipment is under development to fit commercial manufacturing purpose. Therefore, new or refurbished facilities for this segment need to be flexible, agile and future proof. They also must be extremely good at handling small number of precious batches at a higher frequency to cope with the manufacturing of unique, personalized drugs like CAR-T therapies.
Manual processing is prone to errors and is expensive in operations - in fact, it is said that up to 80% of errors in pharmaceutical production are down to human error.
Staying in compliance: GMP challenges in a personalized medicine world
If you have a cell therapy that you are waiting to put into commercial manufacturing, there are some big decisions to make. For instance, should you build your own manufacturing facility, use a CMO, or perhaps lease a cleanroom container until processes and equipment are developed further? Whichever option you choose, the first step on this evolutionary journey is to consider the GMP implications and implement a strong control strategy.
Manufacturing autologous therapies requires aseptic manufacturing suites, which means high GMP classification during manufacturing (unless manufacturing is conducted in closed processes). Additionally, most manufacturing is currently done by manual aseptic processing, which requires highly trained and qualified personnel. And as more therapies for more patients are produced, more manufacturing suites are needed to be able to produce batches in parallel. Instead of ‘scale up’, we need to think ‘scale out’ for commercialization.
The main issue here is that manual processing is prone to errors and is expensive in operations - it is said that up to 80% of errors in pharmaceutical production are down to human error. This percentage hits particularly hard when you consider how these unique therapies use a patient’s own stem cells, so any unplanned shutdowns or faults can result in impurities in the cellular therapy product. This can be life threatening for the patient, particularly in cellular therapy facilities where treatment is often acute.
In addition to this, Annex 1, one of the most comprehensive updates in EU GMP regulations to date, will be finalized this year. Among other things, Annex 1 focuses specifically on a general risk based approach, moving the operator away from the product and making sure manufacturing processes are digitally traceable.
>> Read more on the Annex 1 draft from the EMA
A journey towards closed processes and full automation
So how do we deal with these challenges? Most importantly, we need a change in mindset. Although manual handling still dominates in the development of autologous therapies and the start-up of commercial manufacturing, the potential for product risk and the associated costs of high grade GMP environments logically points towards closed systems like isolators. Isolators are easy to scale out and mitigate cross contamination risk, as “open handling” is performed in a closed primary barrier system.
Short term, this solves many of the above issues. But long term, we need to take this one step further. The FDA guidance on Aseptic processing points out that:
“Automation of other process steps, including the use of technologies such as robotics, can further reduce risk to the product” 1
To substantially lower the risk of operator contamination, the ideal environment would be a fully closed barrier system, no operator in contact with the product, and a robot that conducts all handling tasks. Alongside this, utilizing single-use technology and closed process philosophy would remove the hurdles of cleaning and decrease cross contamination risk
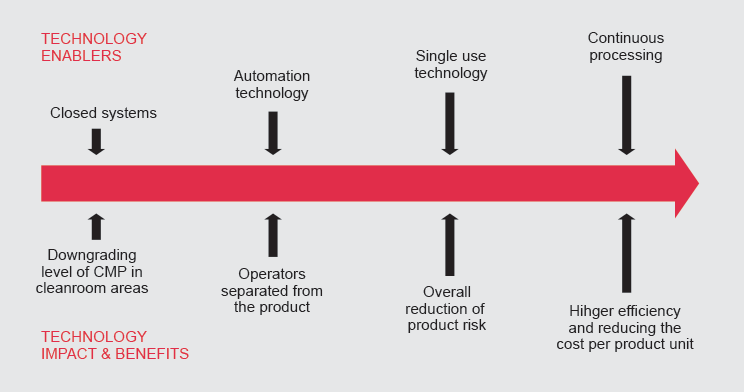
Sustainability benefits: operational cost cutting and an improved working environment
It may not be immediately obvious, but this shift towards closed manufacturing processes has many other positive implications. For example, downgrading the GMP room classification by using closed systems significantly reduces the amount of ventilation needed in a facility. Additionally, if the operator is separated from the product there is no need to go through a full gowning procedure several times a day. Both factors mean lean operations, reduced waste and huge energy savings.
Shifting towards this model will also significantly improve the working environment for the operators themselves. Having to gown up and down several times a day and wear a full GMP Grade B cover suit and mask is a high impact on work environment (plus not being able to go to the bathroom or eat anything for several hours must take its toll). A better working environment means happier employees, which means less stress and less errors . Ultimately, it makes a company a more attractive workplace, and a more attractive option for highly sought candidates within a very competitive industry.
Disruptive innovation in pharma?
Game changing trends such as CAR-T cell therapy are sending waves across the manufacturing industry. ATMP facilities are moving away from manual handling and operators handling products in GMP grade A benches with grade B cleanroom backgrounds, to more flexible facilities with automated processes and operators separated from the product.
Just as disruptive innovation has affected numerous other industries over a short period of time (think LPs to CDs to Smartphones), disruptive innovation also affects pharma manufacturing. Currently the technology does exist - but is not yet available in a convenient “all in one” package. Yet the speed at which innovative technologies evolve has increased at an unprecedented pace, and pharma manufacturing technology is no different. The real question is not “if”, but when and how we will implement the changes.
Finally, to develop these concepts properly there needs to be a joint and coordinated cooperation between pharma engineering consultants, universities and hospitals, equipment developers, pharma manufacturers, CMOs, and regulatory bodies. Ultimately, with a collective effort, what seemed unrealistic only 10 years ago is now becoming a real possibility. With personalized medicine and autologous therapies taking the stage, the future vision of more sustainable ATMP facilities is now in sight.
1 Guidance for Industry: Sterile Drug Products Produced by Aseptic Processing – Current Good Manufacturing Practice, Pg. 10



